How Your Spinal Fusion Impacts Your Pelvic Floor
Welcome back to my blog series on all things spine and pelvis, and how they impact one another! Today I’m diving deep into spinal fusion and pelvic floor dysfunction.
If you’re one of the thousands of people living with a long spinal fusion as a result of your scoliosis, you likely have had to adapt to many changes in how your new body does, and doesn’t, move. For many of us, the most noticeable changes feel like stiffness through your back and ribcage, limited ability to twist and turn around, or needing to learn how to use different muscles when you’re moving, lifting things or even breathing. These movements and the ways we use our body are all impacted by our spine, and spinal fusion literally changes how your whole body can move and function. This, in turn, influences your entire core system - which includes your pelvic floor.
As you may remember reading before in my pelvic floor blog, your core is made up of a whole group of muscles, including the diaphragm, the deepest abdominal and back stabilizer muscles, as well as the pelvic floor. All of those muscles are crucial in how we move, breathe, manage loads, and hold ourselves each day. When part of the system loses mobility (think your spine and rib cage after a spinal fusion), the whole group of muscles needs to adapt.
…And our bodies do a beautiful job creating new strategies and movement patterns to accomplish the many jobs they need to do to stabilize us. However, sometimes these new strategies can create new issues, like:
Feeling of tightness or tension deep in your pelvis
Bladder symptoms
Discomfort with exercise or intimacy
This blog is intended to help you understand why this happens, what changes could be contributing to them, how pressure management and movement strategies can help (or hurt), and how you can support your pelvic floor to feel more confident and strong in your post-fusion body.
Quick disclaimer before we go:
This is a gentle reminder that this blog cannot serve as medical advice. This blog was created for your information only, from an expert in scoliosis, spinal fusion and pelvic health. For individualized or more personal advice you can schedule a complementary clarity call or book a consult or with me for my expert opinion.
How spinal fusion impacts our pelvic floor
In case you’re new to me and my content, you may want to go back and review my blogs describing what scoliosis is, what scoliosis exercise is, or generally how scoliosis impacts our pelvic floor.
In the last blog, I talk in detail about the core canister and all the muscles involved, with a diagram to show how it works. While I highly recommend you go back and read it, here’s the summary:
Our core canister is made of muscles on the top and bottom of the abdominal cavity, surrounded by our deepest core muscles on our front as well as spinal stabilizers. Those muscles, as well as the pressure within it, provide our stability.
In order for those core mechanics to function optimally, it requires:
Coordination of the muscles as we breathe and move
Mobility within our spine and ribs, abdomen and within our pelvis
Dynamic movement as we breathe, ideally with rib expansion in 360 degrees - forward, backward, and sideways
So, right off the bat, at least one of those pillars is directly impacted the second we awake with a new set of hardware in our spines.
An illustrated version of my actual spine complete with hardware -__-
What spinal fusion changes
In just a little bit, we’re going to dive into spinal fusion and the pelvic floor specifically, but let’s start a little more generally on some typical changes that happen in our bodies after a spinal fusion.
Limited thoracic mobility & trunk rotation
Most people with spinal fusion have at least part of the thoracic (or mid back) fused.
Let me give you a little introduction into the mechanics of your spine: different sections of the spine are responsible for different types of movement. In the thoracic spine, the structure of the segments are responsible for most of our trunk rotation. This means, of course, that a spinal fusion into the thoracic spine will definitely limit your ability to twist one way or another.
That rotation that used to come from your spine pre-fusion now has to come from other parts of your body, typically:
Your shoulders
Your hips
The unfused segments of the spine
The change in movement strategies can impact our stability during the movements, can create strain on the structures that are now having to work differently and can absolutely impact our pelvic floor engagement and create tension in it.
Suboptimal breathing mechanics (lack of 360 degree expansion)
As I alluded to above, spinal fusion usually leads to stiffness in the thorax and rib cage, and though the ribs are not fused, the fusion usually impacts their ability to expand in all directions - forward, backward and outward.
As a result, this decrease in the 360° expansion can lead to:
Upper chest breathing and overuse of neck accessory muscles, like the upper traps, scalenes and smaller less efficient muscles
This might present like chronic neck tension or pain, headaches, or feeling short of breath easily with activities
Excessive belly breathing but limited recruitment of the diaphragm (which is our primary breathing muscle)
Changes to the pressure system within the chest and abdomen, which creates more downward pressure on the pelvic floor muscles
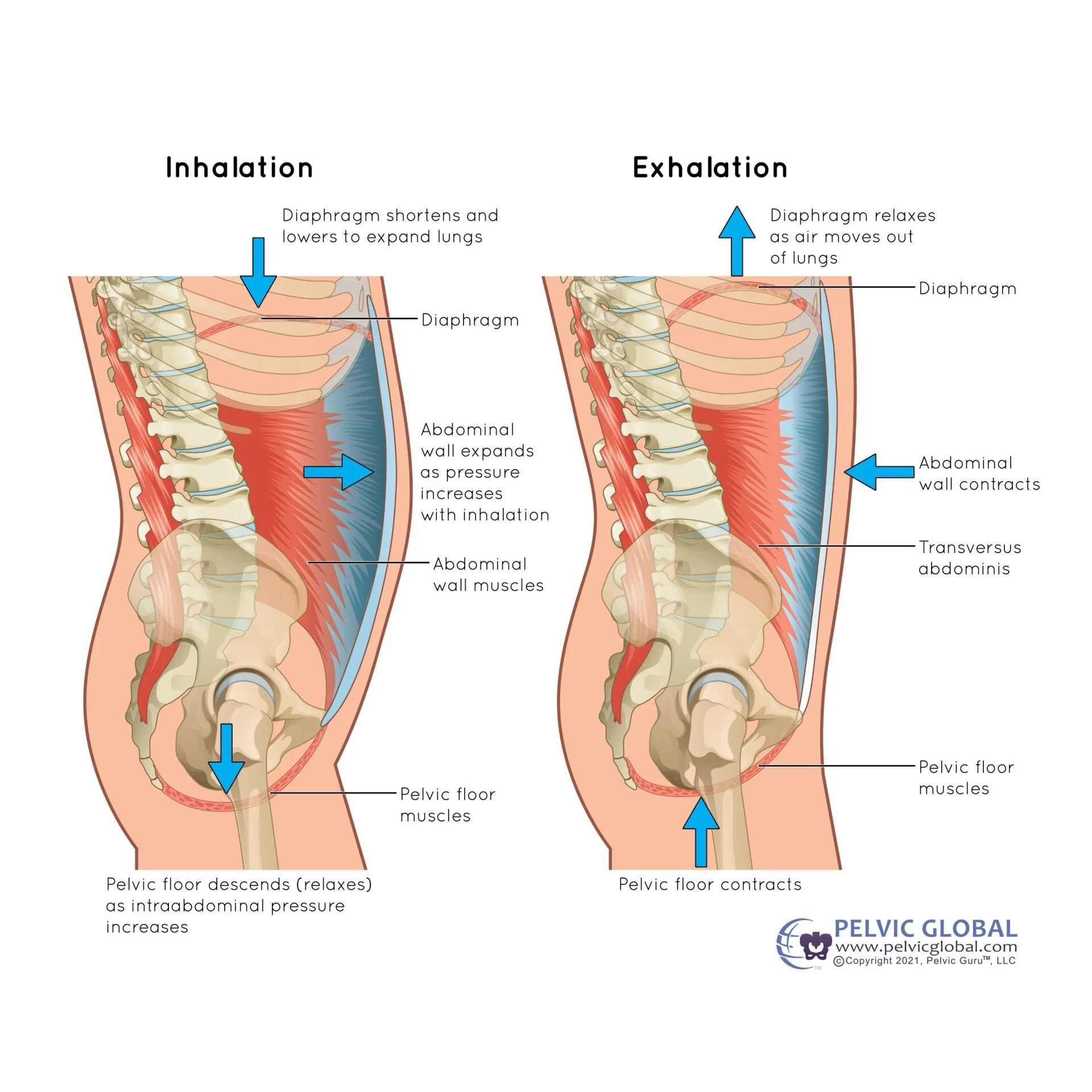
(Need to see it to visualize it? Scroll down to see an illustration of what a natural breathing rhythm typically looks like.)
Cross-section of the body showing the rib cage, the diaphragm and the pelvic floor and what typically happens when we breathe in and out
Joint stiffness & compensatory patterns
With the spine less mobile, the surrounding areas work harder:
The hips and all the surrounding muscles that stabilize it
The sacroiliac joints, a.k.a the SI joints. In case you’re unfamiliar with these and their importance, check out this site!
The cervical and thoracic segments above the fusion
The lumbar segments below the fusion — if there are any!
Some people get fusion all the way into the pelvis bones and don’t have any unfused lumbar segments
The diaphragm and abdominal wall
As our bodies adapt and develop new ways to move and stabilize themselves, we may feel aches or tension in different areas we’re not used to. On top of that, these new movement patterns can impact the alignment of our pelvis and how we distribute loads from our feet up to our heads.
Limited pelvic mobility
On a similar note, we can start to feel more stiffness within our hips and pelvis as it acclimates to the lack of mobility in the spine and ribcage.
We can notice:
Change or decrease in the natural movement we would have in our pelvis during movements like walking, bending over, and exercising
Sense of pressure or general tension or “tightness” in the pelvic floor, low back or hips
How these changes affect the pelvic floor
Okay, so you’re made it this far. Let’s get technical about what we can notice in the pelvic floor itself.
Changes in pressure management
Pressure management is an area that can impact all of us, and is also one of the most common ways a spinal fusion can change how the pelvic floor can function. As I mentioned earlier, the core is one giant pressure system with muscles surrounding the abdominal cavity. That intra-abdominal pressure is a huge component of how we stabilize our bodies during our daily activities.
When the system is working as designed, there should be natural movement in all of the surrounding muscles as we breathe, sneeze, cough, lift or exercise. This coordination helps us breathe easy, manage pressures outside and inside of us, and stabilize the spine.
After spinal fusion we experience changes in that natural movement and rhythm. The lack of mobility in the spine limits the amount of rib movement we experience, translating into less expansion of the diaphragm. To compensate, the effort of breathing must shift upward or downward, and that lack of expansion means that internal pressure has fewer places to move and expand. The pelvic floor is a natural backup primed to accept that load.
Over time, that altered pressure management can lead to:
Feeling of constipation or needing to strain when trying to pass a bowel movement
Heightened urgency to pee or leaking with activities that increase pressure in the abdomen (think coughing, sneezing, high impact activities or weight lifting)
Sense of pelvic floor tension, gripping or muscle overactivity
Pain or discomfort with exercise - particularly when holding your breath or “tightening your core”
Changes related to sexual activities or intimacy such as:
Discomfort or pain during penetration
Sensitivity or irritation anywhere in the genital region
Inability to climax, feeling “stuck” or plateaued
Pain or leaking during climax
Discomfort, soreness or pain for any amount of time following intimacy
Difficulty relaxing the muscles within the pelvis
If any of these symptoms sound all too familiar, don’t worry! You can learn better pressure management strategies with a little assistance.
Pressure management and how we do it is highly individualized and it can be tricky to make general recommendations without assessing what’s going on first, but I do speak a little more detail into what “normal” mechanics of the breath and muscle activation look like in the pelvic floor blog, in case you want to check that out and come back!
You can train your diaphragm and muscles in your rib cage to get more outward and backward expansion (as much as is available to you) to reclaim more mobility and movement within your rib cage. As we regain a more natural movement and rhythm in our ribs and below, even that alone can sometimes take the load off of the pelvic floor muscles, easing our symptoms and improving our movement and stability strategies.
Pelvic floor overactivity, a.k.a. gripping
For all of the above reasons, we can become much more aware of those muscles deep down in our pelvis after a long spinal fusion. Altered movement strategies may depend on the pelvic floor muscles to stabilize us more than they did before, plus the lack of mobility within the spine and rib cage can put more stress on the pelvic floor. As I mentioned before, the muscles within the pelvic floor are a natural back up when other muscles or strategies aren’t working to keep us stable (or mobile).
In other words, the muscles are being used more frequently, for more tasks, and aren’t getting the chance to cycle between contracting and relaxing the way they were designed to!
We may notice the gripping during sitting, as well as during more strenuous or dynamic movements. That overactivity alone in the pelvic floor can lead to symptoms such as constant deep hip, pelvic or low back tension, more urgency to pee, constipation or issues pooping, trouble during sexual activity or pelvic pain.
Changes in alignment and center of balance
Before your spinal fusion surgery, your body and your brain were accustomed to a certain posture and alignment (how you held yourself) — and after, your surgeon used hardware and equipment to literally reshape your spine and its alignment!
This sudden change of body position can be quite disruptive to your sense of balance and how you use your postural muscles, which include your core muscles (of course), but also the large muscles in your legs, and the spinal stabilizers up into your neck.
Those alterations in pelvic tilt and rotation stemming from the spinal fusion can impact:
Muscular effort & balance around the hips
From front to back or from side to side
Patterns of tension throughout the postural muscles
How the load is distributed throughout the pelvic floor muscles
Increased movement demands
Due to the lack of movement in the areas affected by the fusion, many large movements such as bending down, lifting up heavy items and twisting are now largely dependent on the hips and pelvis. If our core strategy isn’t working efficiently, the pelvic floor will need to “pick up the slack”. With all of this in mind, it’s no wonder why spinal fusion can lead to pelvic floor dysfunction!
What changes did you notice in your pelvis after spinal fusion?
|
What changes did you notice in your pelvis after spinal fusion? |
So now you know that yes, your pelvic floor is impacted by your spinal fusion. If you now find yourself wondering what to do about it, I’d suggest reading my blog on how you can support your pelvic floor with scoliosis or spinal fusion.
Questions? Drop me a comment below, send me an email or book a complementary 15-minute clarity call and let’s get things sorted out!
Also, make sure you’re following me on Instagram for more quick tips and insights, and join the newsletter family for all the updates on ways to support your spine and pelvic floor!