What Is The Pelvic Floor?
The pelvic floor muscles are a group of muscles that sit in the bottom of your pelvis bones. Some describe them as a sling, or hammock, that supports your pelvic organs - your bladder, your uterus and ovaries (if you have them), and your rectum. They play several roles in our body including:
Sphincter control - keeping our pee or poop in until we are ready to release them)
Stability - working with our deepest core muscles
Support - holding our pelvic organs in place
Sexual - playing a role in arousal, sexual activity and climax
“Sump pump” - lymph management out of our legs
These are commonly known as the 5 “S’s” of the pelvic floor. I’ll get into a little more detail below. Keep reading…
A little disclaimer before we go on: please remember that this blog is solely for your information from an expert in scoliosis, spinal fusion and pelvic health. That said, this blog and everything within it can not serve as medical advice. Remember each person will have different circumstances and you should discuss your own with your personal medical & wellness team, or you can book a consult with me for my expert opinion.
Depending on how we describe them, we can also envision the pelvic floor as a trampoline. When working as designed, the muscles provide a little bounce, or give, to support us from below when we’re moving throughout our day. They also squeeze to stop you from leaking, and also squeeze involuntarily when our bodies experience a sudden unexpected pressure - like a sneeze or cough.
They also act as a gateway at the bottom of your pelvis. The muscles can open or relax, allowing us to pee, poop or pass gas. For those of us with vulvas, those muscles must also relax to allow something in, such as a speculum, a penis or another penetrating object. On the other hand, those muscles must also remain closed when we are trying to keep something in. These muscles are somewhat unique to other muscles throughout our body as we have both voluntary control (meaning we can control how they work) and also involuntary control. That means they will react without us having to think about or do anything!
Finally, they also play an important role in our core stability - they are literally the floor of our core! There’s a popular model among physical therapists and movement pros that describe our core as a canister, or cylinder.
Check out this gorgeous picture of the female pelvis, complete with pelvic floor muscles! In this view, you are looking from the bottom, with the front of the pelvis being at the top and the spine and sacrum bones at the bottom.
This is how it breaks down:
The diaphragm is top of the can - our main breathing muscle that spans the width of our ribcage and divides us into an upper and lower half
The innermost abdominal and back muscles (namely, the transverse abdominis and the multifidi - the deep muscles that support & connect each segment of our spine) are the walls of the can
The pelvic floor muscles make up the bottom of the can
All this in mind, the pelvic floor muscles must work in concert with the other muscles within this core canister in order for us to be able to run, jump, lift heavy things, or pick up our children. Healthy, functional muscles are supported by connective tissue (also known as fascia), as well as the nerves of the pelvis and the bones.
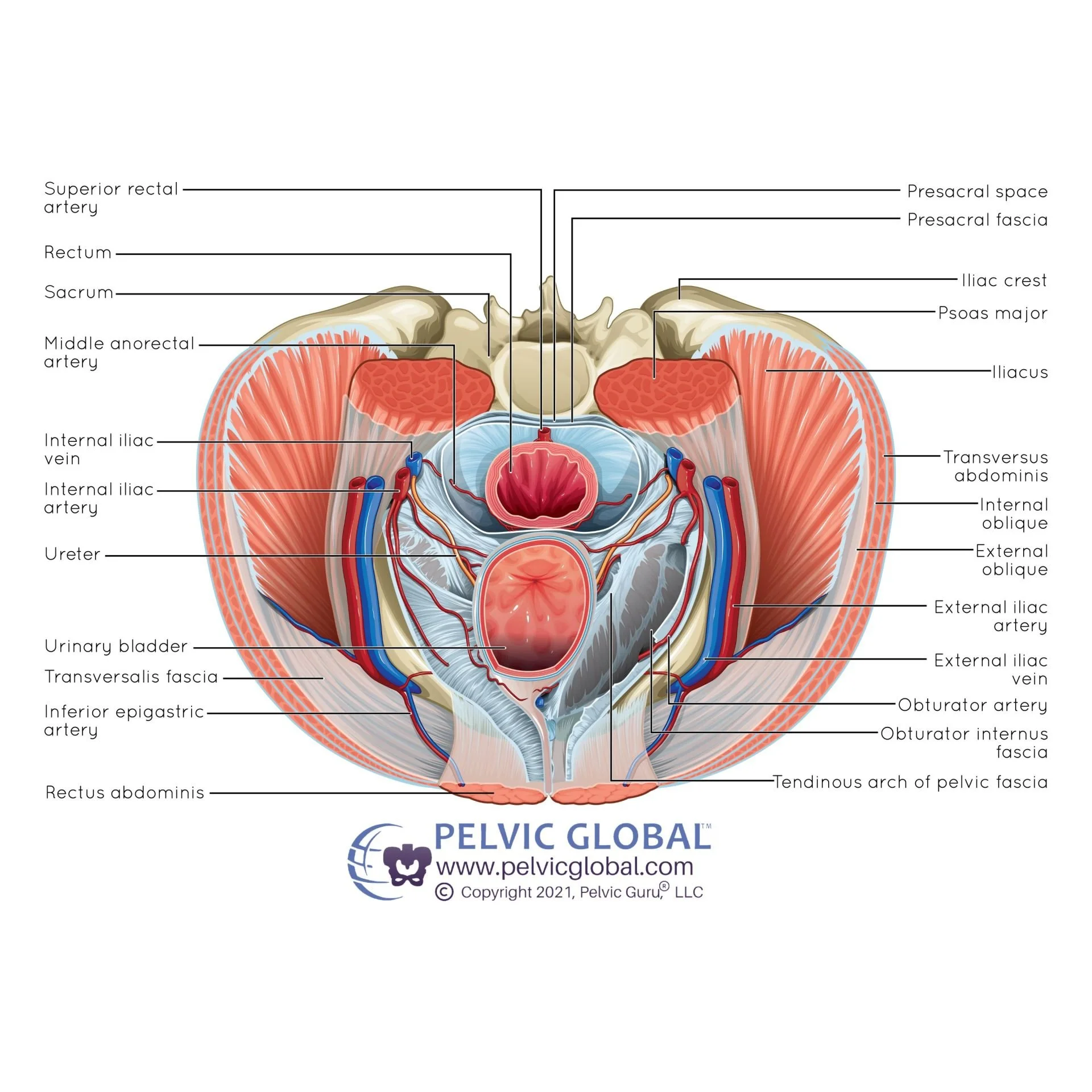
Here’s a view of the male pelvic floor from above (yes, men have a pelvic floor too!). At the top of this picture you see the spine bone and the back of the pelvis, below it is a cross-section of the rectum and the bladder below it.
Still having a hard time picturing how this muscle coordination works? Check out this video of how to coordinate your pelvic floor with your deepest core muscles!
When the pelvic floor works well
When our pelvic floor muscles are working well, we often don’t notice them at all. I tell my patients and clients that if you’re unaware of your pelvic floor muscles, that’s likely a good thing! Healthy, well coordinated pelvic floor muscles are able to do all of their jobs well without any issues.
A well-functioning pelvic floor may mean you can:
Make it to the bathroom when you’d like, without fear of an accident
Sneeze, cough, run, jump or lift heavy things without pain, pressure deep in your pelvis or leaking
Comfortably wear a tampon or enjoy intimate experiences, partnered or solo
Exercise without leaking or feeling heaviness or discomfort in your low back or genital region
Move easily without worrying about pelvic pain, leaking, or pelvic heaviness
When things aren’t working well (aka pelvic floor dysfunction)
Sometimes and for a variety of reasons, these muscles can struggle to perform all of their many jobs well. The medical & therapeutic phrase for this is pelvic floor dysfunction. In some cases, that struggle may feel subtle (like pelvic heaviness, constipation, frequent need to pee or increased urgency to pee), and sometimes the signs are more obvious.
That can look like:
Leaking pee or stool
Passing gas involuntarily
Pain during intimacy
Severe constipation (feeling like there’s something there but you can’t get it out)
Pain during or after pooping
I shouldn’t go much further before telling you pelvic floor dysfunction can be complex to work through. Remember that these muscles work as a part of a system - controlling your pressure management, your core stability and athletic performance, your ability to keep continent, and so on. Plus, they are affected by the strengths (or weaknesses) from all the muscles around them - including the glutes, the hip stabilizer muscles, the core and the spinal muscles. They also may be impacted by other factors, such as restrictions in scar tissue from abdominal or back surgeries. If you have scoliosis or spinal fusion, that can impact how your pelvic floor functions too. The pelvic floor can seem like the culprit when things go wrong, but more often it is the victim of the circumstances.
The muscles may be overly weak, such as after an abdominal or pelvic surgery, or after childbirth. They could be overly tight, or overactive, like a trampoline that’s been pulled too tightly that doesn’t have much give. It’s also possible that the muscles are both tight and weak. Because this particular set of muscles work in so many ways and as part of a system, it’s helpful to have a skilled person on your team who can assess you as a whole and give you personalized advice to help in your specific circumstances. (And if you don’t have anyone locally you can trust, remember I can see you virtually.)
While pelvic floor dysfunction is common, it’s not normal, and you can get help. We live in a culture in which leaking, pain and pelvic issues have been normalized. However, knowing what’s “normal” and what isn’t is a powerful first step in finding a solution for our issues! Pelvic floor dysfunction can really impact our quality of life, so if you’re struggling with it, please know you are not alone and there is help available.
What if I’m having issues with my pelvic floor?
Dealing with pelvic floor dysfunction can be very stressful - particularly if you’re feeling out of control or leaking. It’s also more common than you might think: almost 1 in 2 women (45%, to be more precise) will experience some form of pelvic floor dysfunction in their lifetime, and 15% of men will too.
If you’re having issues with your pelvic floor such as leaking, pain, heaviness, constipation, or sexual issues, you may benefit from seeing a specialist trained in evaluating and treating the pelvic floor muscles. In most places in the world, that may be a physical therapist (or physiotherapist), occupational therapist with advanced pelvic floor training.
That said, there are certain signs that you may need to see a doctor first. Here’s a list of RED FLAGS to look for:
Sudden change in bowel or bladder function
Losing full control of your bladder
Inability to feel a full bladder or rectum
Significant change or increase in pain in a short time
Severe numbness, tingling or weakness in the groin or down the legs
Frequent or chronic urinary tract infections (UTIs) or yeast infections
If any of those are present, get an exam from a doctor like a primary care provider, who may refer you to a urologist, a neurologist or other specialist to clear any other conditions or issues.
Next steps…
If any of this is ringing true for you, here are some next steps to explore:
If you do have curvature in your spine, read this blog about how scoliosis can impact your pelvic floor muscles
Find a pelvic floor therapist near you for an evaluation
Not able to find or access a pelvic floor therapist? I created a free guide to assess your own pelvic floor muscles.
Note: While this is not a substitute for pelvic floor therapy, it does give you some insight as to where you are now and some guidance on what should be happening
Schedule a complementary 15-minute virtual call with me to get more specific guidance or send me an email with your questions. And, as always, you can book a virtual consult with me to get expert advice on your situation from anywhere in the world, from the comfort of your own home.
Wrapping it up
Your pelvic floor is a complex, dynamic and powerful group of muscles that play many important jobs, and though sometimes challenges happen you can regain harmony in your pelvis! Having the right tools can make a world of difference.