How to Support Your Pelvic Floor with Scoliosis or Spinal Fusion
If you’re one of the thousands of people worldwide living with scoliosis or spinal fusion, you may have heard of these muscles before, or you may not have any awareness of this whole region of your body. For those of you living here in the U.S, this topic may feel shameful or taboo to talk about because of the type of culture we grew up in. You might even not think much about your pelvic floor until you experience some new or unexplainable issues — maybe you notice a little leaking when you laugh or cough, trouble going to the bathroom, needing to pee a lot more than you used to, a heavy feeling in your low back or “down there”, or even pain during movement.
Why you should be interested in your pelvic floor with scoliosis or spinal fusion
For those of us living with scoliosis or spinal fusion, we may be more prone to issues with these very unique muscles, and that can show up in unexpected ways. When the spine curves or moves differently, it can change how the pelvis sits, your breathing patterns, and even the alignment and ability of the pelvic floor muscles to work as designed. Building awareness of and reconnecting to these muscles can be life-changing, and can help you feel more stable and in control — from walking to exercise — feel steadier and more comfortable.
If this is the first blog of mine you’ve come upon, you may want to go back and read some of the others in this series, such as:
I’d recommend going back and reading them ahead of time to answer any questions that may come up as you keep reading - but don’t worry, I’ll also link them at the end for you!
How scoliosis may create (or worsen) pelvic floor dysfunction
To summarize, scoliosis can create a number of different demands on our pelvis, and also our pelvic floor muscles. Here are 5 ways a scoliosis curve — or more than one — may impact the pelvic floor muscles
Shifting, twisting or tipping of the pelvis can create asymmetrical, or uneven, forces on the pelvic floor muscles. Meaning, one side of the pelvic floor may be bearing more stress or load than the other. This could lead to leaking, or pain deep in the pelvis, the groin, hip or low back (particularly with exertion or certain types of movement).
Since the pelvic floor muscles were designed to work in concert with the other core muscles, those muscle imbalances caused by the scoliosis may create more tension or force on the pelvic floor, which then has to compensate - or work harder or in unconventional ways.
As the core gets shifted and rotated with scoliosis, it creates changes in our internal pressures - namely, the intra-thoracic and intra-abdominal pressures that help stabilize us. This change in pressure systems can result in compensatory breathing mechanics and alter our muscles that work to support us. These shifts can lead to more downward pressures on the pelvic floor, which could lead to overactive muscles and may contribute to pelvic organ prolapse, or descent of the pelvic organs into the vaginal opening (for vulva owners).
If you have a lumbar curve, the torsion from your spine could impact how food and waste moves through your gut - leading to slower motility, more bloating and constipation. Chronic constipation and straining to pass stool can also lead to overactive pelvic floor muscles and can increase your risk for pelvic organ prolapse over your lifetime.
A 2025 study suggested that participants with larger scoliosis curves was related to issues with bladder issues and pelvic floor concerns. As usual with scientific studies, more research is needed.
On a personal note, I want to gently remind you that just because there may be a relationship between scoliosis and pelvic floor dysfunction, doesn’t mean there is a guaranteed link, nor that you will have issues if you have a larger curve. This particular study, though its title is powerful, only studied 12 adolescent girls at one clinic. You may have heard this phrase before, but remember correlation is not causation — meaning the presence of a relationship doesn’t mean one thing caused the other: only that there is a relationship.
That said, scoliosis is rarely the only cause of pelvic floor dysfunction on its own. There are other research studies that haven’t found a direct link between scoliosis and pelvic floor symptoms, like this 2016 study investigating the cases of over 1500 women.
The purpose of this blog
In this blog, I’m going to break down a few actionable, evidence based steps you can take to support your pelvic floor with your scoliosis or spinal fusion in mind. We’ll discuss how even the most basic changes you can make in your habits, breathing mechanics and movement strategies can help these muscles work more effectively and efficiently, regardless of:
Your age
The type of curve you have or how big it is
How long you’ve had scoliosis or spinal fusion
How long your fusion is or how many surgeries you’ve had
How long it’s been since your spinal fusion
In case you haven’t seen my other blogs, here’s your friendly reminder that this blog is solely for your information from an expert in scoliosis, spinal fusion and pelvic health; therefore this blog and all the information contained within it can not serve as medical advice. Remember each person will have different circumstances and you should discuss your own with your personal medical & wellness team, or you can book a consult with me for my expert opinion.
On how breathing impacts the pelvic floor
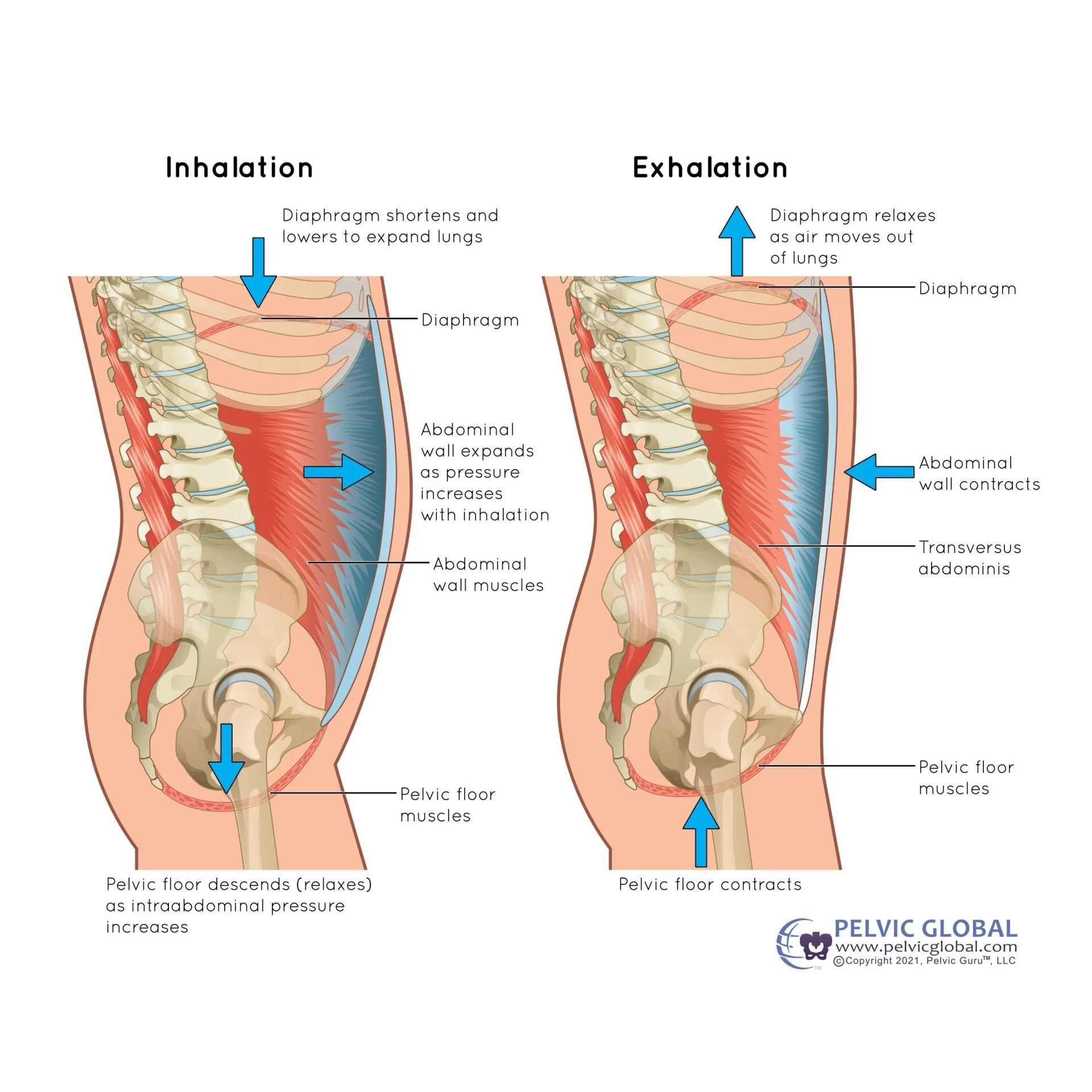
If you already read the blog on the pelvic floor, this will be a review for you but in summary: your pelvic floor should be moving and responding to your breath. Your pelvic floor should be gently lengthening, or going down, when you breathe in and returning to resting position when you breathe out.
One big change we can see in people who are living with scoliosis and spinal fusion is that our breathing patterns can change, often becoming:
Shallower & more frequent breathing rhythm
More driven by our upper chest and neck muscles than our diaphragm (what should be our primary breathing muscle)
Less expansive due to stiffness in the ribs
Check out this graphic on how the pelvic floor should respond to our breath, courtesy of Pelvic Global.
How breathing changes can impact your pelvis
When your breathing feels restricted or harder because of a scoliosis or spinal fusion, it can manifest itself in any number of ways below the belt.
For many people, it just feels stiff or “tight” all the time. It may not create any specific issues other than that…
That said, a stiff and non-moving pelvic floor is more prone to:
Leaking while coughing, sneezing, running or jumping
Having a harder time passing a BM (a.k.a bowel movement) because the pelvic floor struggles to lengthen, or relax
Difficulty with intimacy, feeling unable to climax or being very sensitive in the genital region
A feeling of heaviness in the pelvis or genital region, almost like you’re sitting on a golf ball or you have a tampon inserted
This could manifest as pain during or after a BM or intimacy
Sometimes it appears as deep low back, hip or genital pain with explosive movements, like jumping, lifting heavy loads, or high impact exercise
These are some examples, but of course they may or may not match your experience.
Optimizing breathing for a happier pelvic floor
After reading all of this, you may be wondering if there’s anything you can do about this, and the good news is — you can! Here are some general recommendations to work on as you explore unlocking your ribcage with your breath.
Expanding your breathing in 360 degrees
Think of your ribcage as a ball or balloon: the ribs should be opening in all directions.
Forward, or pressing your breastbone and chest open
Outward, or pressing the ribs out wide
Picture breathing into your bra line or the seams of your shirt)
Backward, or opening your back ribs toward your seat or the floor
Your pelvic floor is happiest when that healthy movement is there as you breathe! Even if you can’t do it all day, try to work this expansive breathing into your day for at least 5 to 10 minutes as often as you can.
Bonus: untwisting your ribs with your breath
If you have a thoracic, or upper back, curve, you likely also have some rotation (twisting) in your ribcage. The best way to tell is to stand shirtless in a mirror and pay attention to which ribs you see more easily. If you have a right thoracic curve, you will see the left front ribs more easily — usually one or two ribs will poke out more than the other side.
When you figure out which side sticks out more, you can assume that the opposite ribs are more compressed, or flatter, on the front. Then you can take a picture of your back and you will see that the opposite is true on the back: the side with the curve has more visible ribs, and there will be some flattening or compression on the opposite side.
Once you’ve identified which way your curve goes, you can try to untwist your ribs by channeling your effort of breathing into the sides that are more compressed, or closed.
So that would look like:
Front right ribs and back left ribs, if you have a right thoracic curve
Front left ribs and back right ribs, if you have a left thoracic curve
Yes, you can isolate how your breath moves!
If you’re willing to give this a try, I’d recommend lying on the floor and placing your hands on your lower ribs. Try to breathe into the ribs, allowing your neck and shoulders to be still (as they often try to compensate, or turn on to help). Focus your breath into the front first, aiming to press those flatter ribs toward the ceiling with your breath.
As always, if this is confusing or you don’t understand how this works, you may want to schedule a virtual consult with me so I can help you be successful with it.
Some other ways to support your pelvic floor
Working on pelvic floor & core coordination
Our pelvic floor should be working in concert with the rest of our core muscles. Taking some time and making sure you can contract the pelvic floor with your deepest core muscles can help make sure you’re able to activate the pelvic floor at the right times. Check out this video where I talk you through the movement, without movement and also with some basic movements added in.
Other types of movements to prioritize that can pay in dividends when it comes to your pelvic floor are:
Bird dogs and gentle core activation, particularly when paired with breathwork
Glute bridges,
Single leg balance exercises
Squats in all varieties
Make sure you are avoid high-pressure Valsalva maneuvers (like breath holding and straining), and play with using your breath differently during effort. Some people prefer to breathe out with exertion and others prefer to inhale. Find what feels good for you!
Other considerations to have a happier pelvic floor during your movements include modifying heavy lifting technique, using an external or internal pelvic support, and using shoe orthotics or heel lifts if there’s a leg length difference or significant pelvis asymmetry.
Prioritizing digestive health
A healthy, functional gut and good bowel movements are crucial in maintaining the delicate balance in our pelvis. When we have chronic constipation, or issues passing our stool, it can literally weigh our pelvic floor down, leading to:
Excessive muscle tension, which can feel like pressure or discomfort in your deep low back, hips or genital region
Overactivity in the muscles
Pain with passing gas or during or after a BM
Higher risk of leaking pee (due to more pressure on the bladder)
This is a very common thing to struggle with; in fact, up to 15% of the global population struggles with chronic constipation!
As some of my mentors in the pelvic health world say: “assume someone is constipated until proven otherwise.”
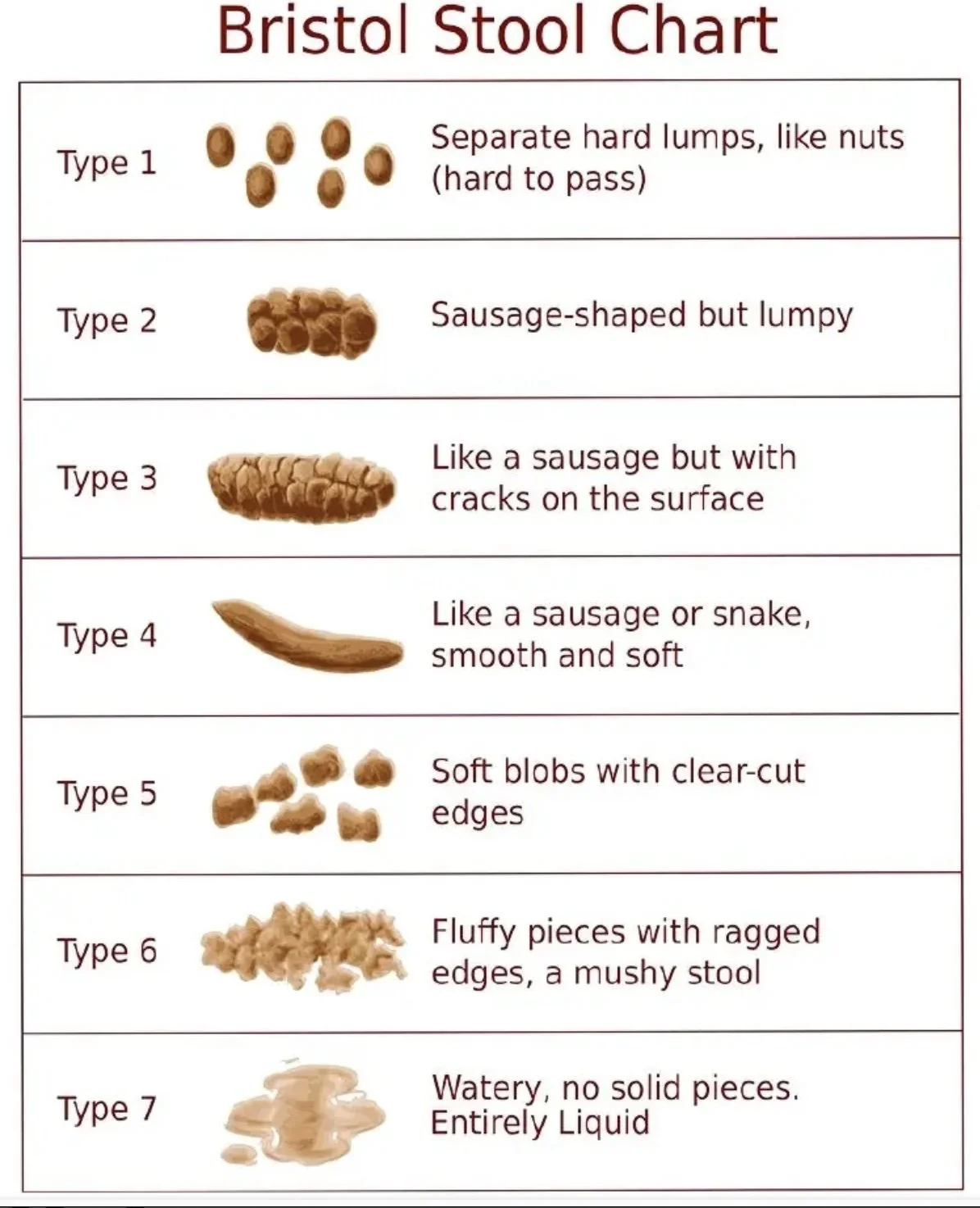
So what is normal for pooping??
Great question! Ideally we are emptying our bowels at least once a day or every other day. Those poops should be solid, smooth or slightly lumpy, and easy to pass. We should feel as though we’re emptying all the way (not like something is still there that we can’t pass), and we shouldn’t feel any pain before, during or after passing the poop.
There’s a chart that shows us the different types of poop, called the Bristol Stool Chart. In case you haven’t seen it before, here it is:
Aim to get Type 3 or 4 stool consistency! The more regular and smooth our poops are, the happier our pelvic floor is!
Are you looking at your poops?
|
Are you looking at your poops? |
Other lifestyle tips for digestive & pelvic health
Hydrate! Aim to get about half your body weight in ounces of water each day.
Eat the rainbow! A well balanced diet containing a good variety of colors and textures ensures your body is getting all the nutrients it needs to function at its best. Don’t forget:
Fiber - think leafy greens, legumes, whole grains and oats
Fruits & vegetables - fresh is optimal, frozen is next best, followed by canned
High quality protein - plant based are easiest to digest & include beans and nuts; otherwise chicken, fish and other types of meat
Healthy fats - such as avocado, olive oil, chia seeds & flaxseed, nuts
Prioritize your sleep. Yes, good quality sleep
Practice regular stress management. When we are constantly feeling stressed, our nervous system can feel stuck in “fight or flight”, which makes it harder for our parasympathetic, or “rest and digest” system to take over. This can be yet another barrier to having a good poop!
Get daily movement! Walk, ride a bike (stationary or regular), swim, do a group fitness class, have an impromptu dance party in your living room … a little healthy movement each day helps to keep our gut moving well and our poops moving freely!
If this is an area that seems daunting, I’d recommend reading my blogs on enjoying exercise with scoliosis and structuring your strength routine with scoliosis or fusion. The second blog has general categories of exercises to be sure to include in your routine to get you started!
But what about kegels??
Okay, some of you may have already noticed, but one thing missing from this list is the regular practice of pelvic floor muscle contractions, also known as kegels. I have a whole separate blog dedicated to kegels and why I don’t usually recommend them for the people I work with. The bottom line is: chances are you wouldn’t benefit from doing regular kegels unless you have recently given birth or had abdominal or pelvic surgery. I highly recommend reading the blog on kegels if you have more questions about it!
What to do if you’re having pelvic floor issues
As you read through this blog series, you may be realizing that there’s some work to do. If that’s true I hope you’ve also learned that you can work with a pelvic therapist to address a lot of it!
Seek help from a trained pelvic therapist for:
Leaking of pee or poop
Inability to control (or pass) gas
Pain with movement or surrounding sexual activity
Here’s what I’d recommend if you are having issues like pain, leaking, constipation or pelvic heaviness -
Schedule a complementary 15-minute clarity call with me to get my expert insight on what your best next steps are.
Find a local pelvic floor therapist who has advanced training in assessing and treating the pelvic floor muscles.
Depending on where you live, you may be able to find a local scoliosis specialist who can teach you corrective exercise for your specific scoliosis curve. If you don’t have a close local option, I can work with you virtually!
A randomized controlled trial from 2024 suggests that using scoliosis exercise can help decrease rotation forces on the pelvis, particularly when combined with other exercises.
When to seek more urgent help
Lastly, here are some RED FLAGS that warrant a visit to your doctor:
A sudden severe change in bowel or bladder function
Severe leaking like full bladder losses
Change in your ability to feel if you need to pee or poop
Onset of numbness, tingling or weakness in the groin or legs
Big uptick in pain or change in quality of pain
Frequent or chronic urinary tract infections (UTIs) or yeast infections
If you’re experiencing any of the above, you may want to check in with your general practitioner or primary care doctor, urologist, gynecologist or GI doctor first to rule out any other more serious concerns.
Final thoughts…
I hope after reading this blog you’ve learned that there actually are some things you can do to support your pelvic floor with scoliosis or spinal fusion! If after reading this you’re thinking you need more help, send me an email or book a complementary clarity call to get more answers to your questions. You can always schedule a virtual consult with me to get more individualized help.
Remember - just like not every curve or fusion is the same, neither is everyone’s pelvic floor! You may need to work on movement strategies or habits, you may need pelvic floor muscle training, or you may need different types of exercises to help restore the harmony between your spine and your pelvis. Sometimes weakness or imbalance in the hip stabilizer muscles like the glutes or core could be creating more tension or work within the pelvic floor.
That said, it’s also important to remember that just having scoliosis or spinal fusion doesn’t mean you also have pelvic floor issues! Check out this study from 2016 that didn’t find any association of spinal curvature with pelvic floor symptoms! Just because they could be related, doesn’t mean that those issues are inevitable!
Sources:
Meyer I, McArthur TA, Tang Y, McKinney JL, Morgan SL, Richter HE. Pelvic Floor Symptoms and Spinal Curvature in Women. Female Pelvic Med Reconstr Surg. 2016;22(4):219-223. doi:10.1097/SPV.0000000000000271
Curillo-Aguirre CA, Gea-Izquierdo E. Effectiveness of Pelvic Floor Muscle Training on Quality of Life in Women with Urinary Incontinence: A Systematic Review and Meta-Analysis. Medicina (Kaunas). 2023;59(6):1004. Published 2023 May 23. doi:10.3390/medicina59061004
Smrcina Z, Woelfel S, Burcal C. A Systematic Review of the Effectiveness of Core Stability Exercises in Patients with Non-Specific Low Back Pain. Int J Sports Phys Ther. 2022;17(5):766-774. Published 2022 Aug 1. doi:10.26603/001c.37251
Talasz H, Kremser C, Talasz HJ, Kofler M, Rudisch A. Breathing, (S)Training and the Pelvic Floor-A Basic Concept. Healthcare (Basel). 2022;10(6):1035. Published 2022 Jun 2. doi:10.3390/healthcare10061035
Still have questions? Comment below or send me an email and I’m happy to help!